Being alive requires a never-ending supply of energy. We use up energy every second of the day. The entire purpose of eating is to provide the body with energy. One of the primary functions of the body is to take the food we eat and convert it into a usable form of energy. Most of this energy comes from blood glucose – it’s the most available source of energy for all of the cells in the body. It would be lovely if we had a continuous slow release of glucose into the bloodstream, providing us with exactly the amount of energy we needed at all times – never having too much or too little. But we don’t. We have other things to do all day than slowly eat every minute to regulate our blood glucose. So we eat in bursts. By nature, these bursts of food create an immediate excess of energy in the bloodstream – more than we need at that moment in time, so we have a system designed to store that excess for future use – when we are no longer eating and our short-term stores start to run low This entire system of energy regulation is run by insulin. Insulin’s job is to funnel excess energy into the cells for future use, then allow it back out when that future comes.
When this process is broken, it leads to all kinds of metabolic drama. In fact, one of the primary drivers of metabolic disease is insulin resistance. Until we start focusing on fixing this insulin resistance, we aren’t going to be very effective at fixing metabolic disease. And until we start fixing metabolic disease, we aren’t going to fix the excess weight that is the result of the metabolic disease. This is what we spend all day in our clinic working on.
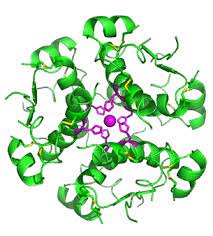
So what is insulin? Insulin is a hormone made by the pancreas – usually in response to excess glucose in the bloodstream. Insulin’s job is to open the doors to the cells so that the extra glucose can enter the cells and be stored. Insulin’s job is to normalize the blood glucose. Insulin resistance occurs when the cells in the muscles, fat, and liver no longer respond well to the insulin signal. Insulin resistance is the primary defect in metabolic syndrome. Although genetic susceptibility can play a part, this problem – this insulin resistance is most often caused by excess insulin stimulation over and over again. When cells get pummeled by insulin molecules day in and day out and they already have enough energy inside of themselves (they don’t need more insulin), they get tired of hearing it and stop paying as much attention.
However, this chronically elevated insulin creates problems. Insulin is supposed to go up and down in response to the blood glucose levels. When blood glucose is high (after eating), insulin is supposed to open the doors to the cells to store the excess. These doors are one-way doors, which is fine when the body is functioning normally. Insulin is up – door swings in – glucose is funneled into the cell. When the blood glucose comes back down (because insulin did its job) the insulin gets metabolized away and the doorway is neutral. A bit later, when the blood glucose drops a little low because the body has been using it, in the absence of insulin, the cells can swing their doorway open the other way and send the glucose back into the bloodstream to raise it. Again, a one-way doorway but functional. It’s a feedback loop. But, when insulin is high and that swinging doorway is stuck in “in” mode and the blood glucose is dropping, you have a problem. You have the glucose inside the cells (you have lots and lots of it) but you can’t access it. So you have to eat again. The body triggers the brain to seek out food to raise that blood glucose.
Think about it this way. In scenario number one, you have a baby sleeping in her crib – in a nice quiet house. All of a sudden the neighbor fires up his chainsaw outside her window and she jolts awake – startled by the noise. She responds acutely/suddenly to the noise. In someone that is insulin sensitive (without insulin resistance), after eating this is how the cells respond to the presence of insulin – they rally up and do their job. Now contrast this with the baby that is sound asleep in her carrier in the middle of a crowded airport. She has learned to accept the background noise and sleep through it anyway. She sleeps straight through the talking and hollering and suitcases being rolled right past her. Even when one of those noisy beeping carts drives right by her, she slumbers away – her brain has learned to tune out the noise. This is how the cells respond to someone with insulin resistance. They stop rallying to attention as soon as the insulin molecule is detected – it’s a normal sound that doesn’t trigger acute action.
Insulin resistance isn’t obvious – you can’t see it like you see a broken bone. Rather insulin resistance manifests itself in various ways, which vary from person to person. Some people get high blood pressure and obesity, others get heart disease and fatty liver but no obesity. This is important – you don’t have to have obesity to have insulin resistance. This is a huge blind spot – for everyone, including health professionals. Most health care professionals and treatments are targeting obesity, which they think is the disease. Rather, it’s just another symptom.
Insulin is the big boss – the one with the megaphone, but there are lots of other hormones at work in your body dictating hunger and satiety (the feeling of fullness). One of the other biggies is a hormone called leptin. Leptin is a hormone released from your fat cells (adipocytes) that tells your brain it has enough energy. In other words, it’s OK to downregulate your eating. Ghrelin is the opposite. Think of ghrelin as “growling” – it’s a hunger hormone released from your stomach that tells your brain it’s empty. In other words, ghrelin tells the brain that it’s time to fill the stomach again.
When insulin is working properly, both insulin and leptin balance ghrelin and keep you weight-stable. But when you become insulin resistant, you eventually become leptin resistant (the brain doesn’t perceive satiety) and ghrelin runs things – and you constantly feel hungry.
We have to go upstream and focus on fixing insulin resistance. We have to let the cells of the body hear insulin again. So how do we do this? First and foremost, we need to stop stimulating insulin release over and over again. This is how we prevent insulin resistance in the first place and it’s certainly a huge part of treatment. We aren’t going to get better if we keep bombarding the body all day with foods that stimulate insulin release. We have to change WHAT we are eating. If that’s not enough, we can start working on the smaller levers – the HOW MUCH and WHEN we eat.
As always, if you need me, you know where to find me
Courtney Younglove, M.D.